Recovery requires fuel, and the fuel the body needs for healing is food.
Under the watchful eyes of caregivers at hospitals, rehab centers, nursing homes, assisted-living units and similar organizations, interventions to improve intake and nutrition can happen quickly and on-site.
But once a patient is discharged, nourishment can slide. One way to address this is by developing a meal service program that provides the nutrition people need whether they are discharged to acute care or senior living. Doing so, whether it’s offered for free or for a nominal fee, has been shown to have a big payoff in quicker recovery time and reduced readmission rates.
This is especially true for “patients—most typically in the 55-plus range—who have some form of acute or chronic disease state that causes them to not get adequate nutrition and who are at risk for malnutrition,” says Larry Altier, System Director of Food and Nutrition Services at Lee Health System in Fort Myers, Florida.
Many factors can account for inadequate nutrition and the impact plays out in many ways. “People who are undernourished or don’t eat enough will have a harder time healing,” says Dana Fillmore, Gordon Food Service Healthcare Segment Manager, RD “and they’re at a higher risk for being readmitted to the hospital.”
Reach out and feed someone
The objective of meal service programs, Fillmore explains, is “to stick to the role of general good nutrition, to make eating convenient for people and to make sure they’re not skipping meals. Eating well is key to one’s well-being and ability to heal.”
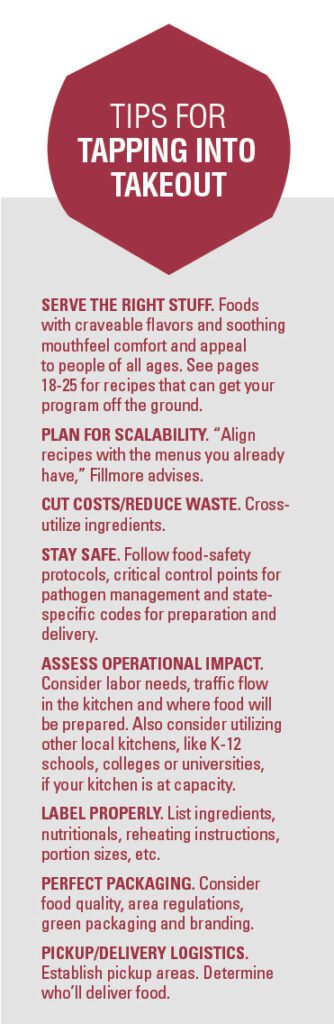
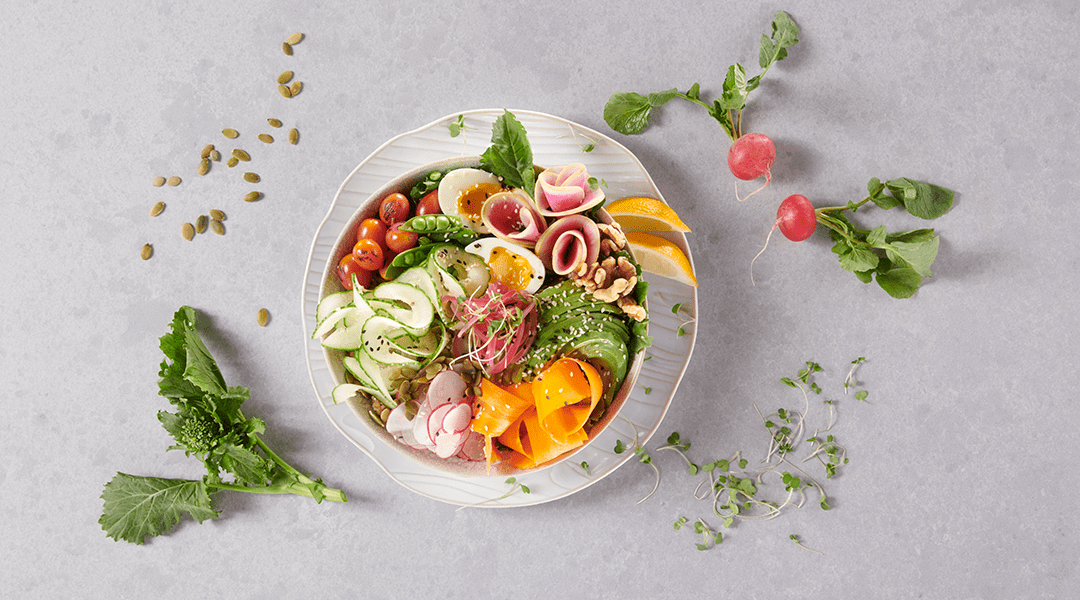
These programs are more UberEATS (an expansion of Uber, the on-demand driving service, UberEATS will pick up your order from a restaurant and deliver it to you) than traditional Meals on Wheels. With Meals on Wheels, meals must follow strict nutritional requirements and organizations are often reimbursed for them. The home meal programs that target this population offer components of simple, tasty meals for pickup or delivery in small enough portion sizes for households with one or two people. The menu can be flexible, anything from prepared in bulk, pre-portioned and provided shelf-stable to fresh and/or frozen.
For individuals discharged from the hospital, a rehabilitation center, or are just in need of some help, this type of outreach overcomes obstacles such as acquiring foods and having to prepare them. For these individuals—especially the elderly—who are not ready for traditional Meals on Wheels or who can’t afford commercial meal-kit delivery, a home meal program facilitates eating, healing and remaining in their homes.
How a home meal program works
The following example shows how a home meal program that is targeted to independent living apartments in a continuing care community might look.
1. Clients place orders in advance, allowing operators to plan for inventory, staffing and workflow needs.
2. Convenience or scratch meals or meal components are prepared and packaged.
3. Pickups occur and/or food is delivered on a set schedule.
Clinically driven and targeted to specific patient needs, Lee Health’s Flavor Harvest at Home program typically serves those ages 55-plus who have some form of acute or chronic disease that causes them to be inadequately nourished. They also must meet two of the six clinical criteria for malnourishment identified by the Academy of Nutrition and Dietetics. Once a week for four weeks, a combination of fresh, frozen and shelf-stable meal components that support their nutritional needs is delivered by a driver who makes sure the food is secured properly in the home. After 28 days, recipients are re-evaluated.
After just 18 months, Altier notes, enrollment eclipses 1,000 participants—and it is well-received. “The first week of the program the recipients are reserved; they barely open the door and keep drivers at arms’ length. By week three, there’s a total change in demeanor, health status is elevated and they open the door and engage with the drivers.”
Even better, the results are positive. “About 59 percent of the patients with similar conditions who didn’t take the meal program were readmitted,” Altier says, “whereas the group that got the meals had a readmission rate below 25 percent. Flavor Harvest at Home had a positive effect from a variety of different measures. This is not just a food program; this is a medical-care program that incorporates food.”
Dining and dollars
Such programs, Fillmore says, offer opportunities to feed the bottom line and improve an operation’s financial health. Moreover, Altier notes, the cost/benefit ratio can be impressive: Lee Health estimated that the cost of Flavor Harvest at “$231,000 and change,” but assessed the net value at “close to $1.3 million, conservatively,” in savings on readmissions and reduced acute-care stays.
Reduced readmissions penalties. “Reimbursed more and more to keep people out of their beds, hospitals are being proactive about improving care by helping with food at home,” Fillmore says. At Lee Health, a significant decline in readmissions yielded significant savings.
Improved Medicare quality ratings. “Because malnutrition is a significantly complicated factor in co-morbidity,” Altier explains, “it has an impact on Medicare mortality or quality ratings for all cases in the system. Improved nutrition can mean no penalties, no increased costs.”
Marketing. It’s important for home meal services to build awareness of who they are and what they offer. Whether it’s a hospital providing meals to discharged patients, a rehabilitation center providing meals to previous clients, a continuing care retirement community offering meals to independent clients or some other form of nutrition care, it sends a positive image to the local community. It builds awareness of who they are and the services they offer.
Narrow networks. “Hospitals are the ones who refer to rehab, skilled nursing and senior living communities,” Fillmore says. “If they’re going to recommend continuing care for a patient, they’ll recommend the one that offers innovative services to keep people healthier longer.”
Sales-driven revenue streams. Fillmore says there may be room “to make money back at minimum and potentially upcharge if you want the program to be revenue-generating.” Whether your home meal program should be free or revenue-generating will depend on the circumstances of your operation. She adds that if you do upcharge, be sure it’s a nominal amount that the target market can bear.
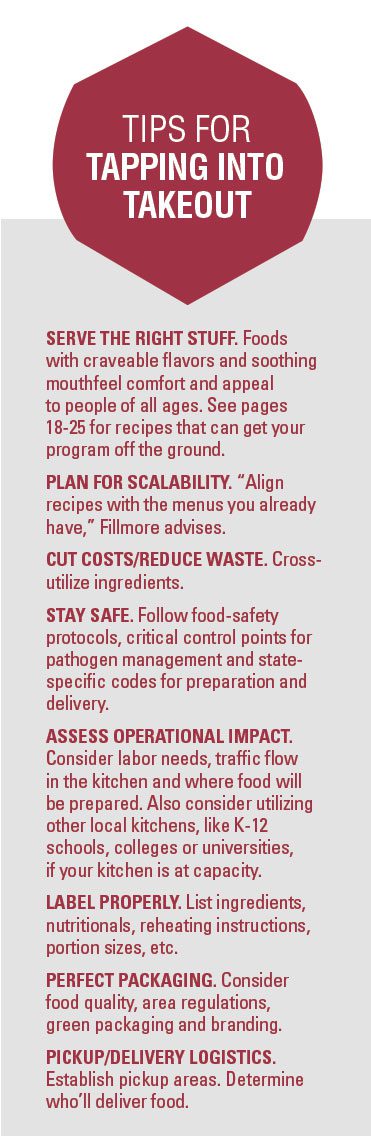
Another option: scale up production even further to offer the meals as takeout fare for employees and/or visitors.
The bottom line? “More and more people will be doing this to reduce healthcare costs,” Altier predicts. “It costs less to feed people for 28 days than to bring them back to the hospital.”
Altier adds that, “better basic care doesn’t get any more basic than nutrition.”
Getting started
The following principles, Altier says, laid the foundation for Lee Health’s Flavor Harvest at Home program.
- Create an institutional culture.
- Redefine clinicians’ roles to include nutrition.
- Recognize and diagnose all patients at risk.
- Rapidly implement interventions and continued monitoring.
- Communicate nutrition-care plans.
- Develop a discharge nutrition care and education plan.
Read more about these principles in the July 2013 Journal of Parental and Enteral Nutrition.
Recipes for a Home Meal Program